TFL denial reasons codes and action plan
CO – 29 – The time limit for filing has expired.
Amerigroup/BCBS of WNY:
Timely filing 120 days from the DOS. Contact Provider Relations to discuss timely filing denials.
HealthFirst:
Children’s timely filing claim guidelines will apply if claim is submitted 180 days after DOS; call account manager for reconsideration of late claims submission.
United:
PI29 The time limit for filing has expired
How to Resolve and Remit/Resubmit
Be sure to know the filing deadlines/ timeframes. Timely filing guidelines are outlined in your contract with the MMCP. Notify your MMCP if there are extenuating circumstances where you do not believe you will be meeting timely filing deadlines for original and/or corrected claim submissions. If possible include reminders in your billing systems as the timely filing deadline nears.
Timely Filing Exceptions
An exception to the filing limit may be requested if good cause is determined CMS defines good cause as
- Administrative error by Medicare contractor
- Retroactive entitlement
- Retroactive MA plan disenrollment
- Retroactive entitlement involving Medicaid
Exceptions may be mailed to NGS before or after the claim is submitted
Preclaim: Completed 1500 claim form, a letter explaining reason claim is being filed late, documentation
Postclaim: Part B Reopening form with documentation
Action Plan:
Identify the Cause: Determine why the claim was filed late. It could be due to internal delays, lack of understanding of payer-specific filing limits, or issues with claim preparation.
Process Improvement: Review and streamline your claim submission process to ensure timely filing. This could involve training staff on payer-specific deadlines, improving internal workflows, or utilizing software that flags claims approaching their filing deadline.
Re-Filing Appeals: If possible, re-file the claim with an appeal letter explaining the reason for the delay. Include any supporting documentation that might justify a reconsideration, such as proof of timely filing or circumstances beyond control (e.g., natural disasters, system outages).
Use of Technology: Implement or upgrade to a robust RCM system that can track claim status, send alerts for claims nearing their filing deadline, and provide analytics for denial management.
Regular Training: Conduct regular training sessions for your team on changes in payer policies, coding updates, and best practices in claim submission.
Authorization denial codes and action plan
CO – 197 – Precertification/auth orization/notification/ pre-treatment Absent. (generally, this means prior authorization was required and was not obtained)
CO -62 – Payment denied/reduced for absence of, or exceeded, pre certification/authorization (generally means Concurrent review requirements were not met).
Amerigroup/BCBS of WNY: For HCBS services, complete the HCBS Provider Notification Form prior to first visit with client and send to Plan.
Example Scenario
Healthcare provider’s office scheduled a patient for an advanced imaging procedure, such as an MRI. The patient’s insurance plan requires prior authorization for such procedures. However, due to oversight or miscommunication within the office, the staff did not obtain the required authorization before the service was rendered.
How to Resolve and Remit/Resubmit
Review manuals in order to determine which services require authorizations and at what point authorization is required (prior, concurrent, etc.). For services that require authorization, please ensure you have reminders in your billing, registration and scheduling systems.
Remember in some instances a denial may be received for services where authorization is not required but Notification is. In these cases. it is important to provide notification so that MMCPs know services are occurring and do not deny the claim.
Detailed Action Plan:
Immediate Response to the Denial:
Recheck the Claim: Confirm that the authorization was indeed missing and not just improperly documented.
Contact Payer: Immediately get in touch with the payer to understand if retroactive authorization can be granted.
Rectifying the Immediate Issue:
Submit an Appeal: If the authorization was obtained but not recorded, submit an appeal with the authorization details.
Request Retroactive Authorization: If the authorization was not obtained, request retroactive authorization, explaining the medical necessity of the procedure.
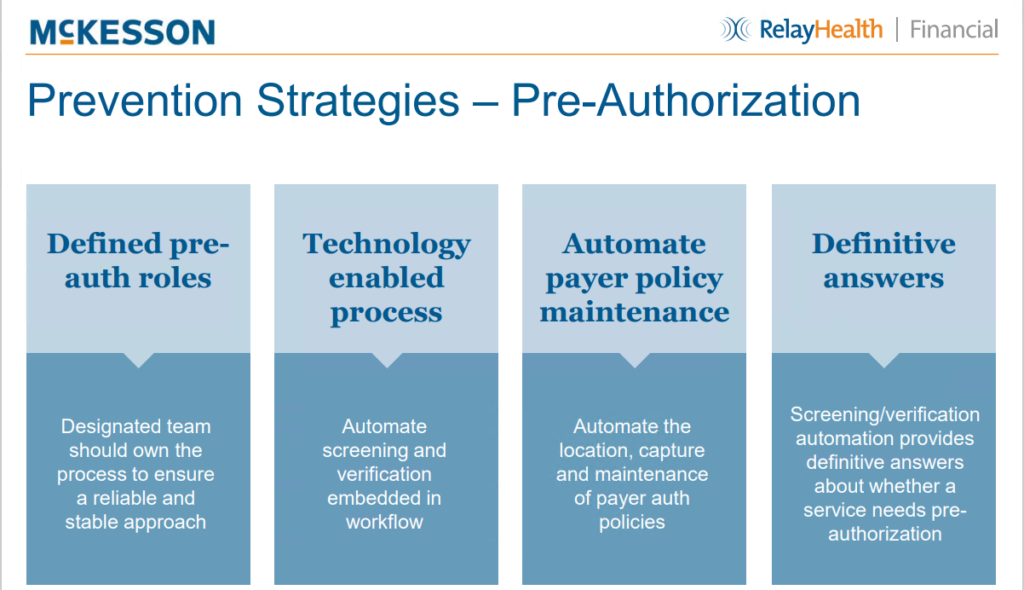
Preventive Measures:
Checklist for Authorization Process:
Process Improvement:
Patient’s insurance details and coverage specifics.
List of services/procedures requiring pre-authorization as per payer.
Documentation of clinical necessity (e.g., doctor’s notes, diagnosis codes).
Deadlines for obtaining authorization before the scheduled service.
Procedure for emergency situations where pre-authorization cannot be obtained in time.
Standard Operating Procedures (SOPs): Develop SOPs for checking and obtaining authorizations. This should include steps like verifying insurance coverage, identifying services needing prior authorization, and documentation processes.
Utilize Technology: Implement an RCM system that flags services requiring prior authorization and alerts staff. Some notification from schedule screen itself.
Documentation and Record Keeping:
Maintain Records: Keep detailed records of all authorizations obtained, including date, time, and the staff member who secured it.
Document Denials: Keep a log of all denials due to missing authorizations to identify patterns or recurring issues.



